Form 1095-B is used to report information about the type of coverage individuals have or had during the tax year. As part of the Affordable Care Act (ACA), also known as Obamacare, the Internal Revenue Service (IRS) requires certain employers, insurers, and other organizations to provide Form 1095-B to individuals who have health coverage.
If you have received Form 1095-B, it’s important to understand what it is and how it affects your tax situation. In this article, we will explore the basics of Form 1095-B and what you need to know.
What is Form 1095-B?
Form 1095-B, Health Coverage, is a tax form used to report information about the minimum essential health coverage provided to individuals during the tax year. It is typically sent by health insurance providers, including insurance companies, government-sponsored programs, and self-insured employers, to individuals who were covered by their health plans.
The form provides details about the type of coverage, the duration of coverage, and the individuals covered under the plan, including the primary policyholder, spouse, and dependents.
Why is Form 1095-B important?
Form 1095-B is important because it helps individuals verify that they had minimum essential health coverage, as required by the ACA. The ACA mandates that most individuals have health insurance coverage or face a penalty, known as the individual shared responsibility payment or the individual mandate penalty.
Form 1095-B serves as proof of coverage and helps individuals determine if they meet the requirements of the individual mandate.
In addition, Form 1095-B is used by the IRS to verify information reported on an individual’s tax return. It is used to reconcile any premium tax credits or other tax benefits that individuals may have claimed on their tax returns with the information reported by their health insurance provider.
This helps ensure that taxpayers receive the correct amount of tax credits and other benefits based on their actual coverage.
Who receives Form 1095-B?
Form 1095-B is typically sent to individuals who were covered by minimum essential health coverage during the tax year.
This includes individuals who have health insurance through their employer, insurance purchased through the Health Insurance Marketplace, Medicare, Medicaid, Children’s Health Insurance Program (CHIP), and other government-sponsored programs.
If you had coverage for the entire year, you will receive Form 1095-B from your health insurance provider. If you had coverage for only part of the year, you may receive Form 1095-B from multiple providers.
What information is included in Form 1095-B?
Form 1095-B contains important information related to health coverage, including:
Covered individuals: The form lists the names, Social Security numbers (or other taxpayer identification numbers), and dates of birth of the individuals who were covered by the health plan, including the primary policyholder, spouse, and dependents.
Coverage details: The form provides details about the type of coverage, such as whether it is individual or family coverage, the duration of coverage (monthly or annual), and the dates the coverage started and ended.
Insurance provider information: The form includes the name, address, and taxpayer identification number of the health insurance provider, such as the insurance company or employer that provided the coverage.
How to use Form 1095-B for your taxes?
When you receive Form 1095-B, it’s important to review the information carefully and keep it for your records. You do not need to attach Form 1095-B to your tax return, but you should keep it as proof of your health coverage in case the IRS requests it in the future.
Read Also: Primerica Life Insurance: Protecting Your Loved Ones’ Financial Future
Form 1095-B Instructions

As a taxpayer, it’s important to be familiar with the various tax forms that you may receive, including Form 1095-B. Form 1095-B is a tax form that provides information about your health insurance coverage. In this article, we will dive into the Form 1095-B instructions, providing you with a comprehensive understanding of what you need to know.
What is Form 1095-B?
Form 1095-B is a tax form that is used by certain entities, such as insurance companies, employers, and government agencies, to report information about the health insurance coverage they have provided to individuals.
The form is issued to taxpayers who are enrolled in minimum essential coverage, which includes most employer-sponsored plans, individual health plans, and government-sponsored plans like Medicare and Medicaid.
Form 1095-B serves as proof of your health insurance coverage and provides important information that you need when filing your tax return, such as whether you and your dependents had health insurance coverage for each month of the calendar year, and whether you may qualify for an exemption from the individual shared responsibility payment, also known as the “individual mandate” penalty.
Understanding the Form 1095-B Instructions
The Form 1095-B instructions provide guidance on how to read and use the information provided on the form. Here are some key points to keep in mind:
Form 1095-B Recipient Information: The top part of Form 1095-B includes information about the recipient, such as the recipient’s name, address, and Social Security number or taxpayer identification number. It also includes the name, address, and employer identification number of the entity that is providing the health insurance coverage.
Covered Individuals: Form 1095-B also includes information about the covered individuals, including their names, Social Security numbers or taxpayer identification numbers, and the months for which they had coverage.
Codes: Form 1095-B includes codes in Part III that provide additional information about the type of coverage that was provided. For example, Code “1A” indicates that the coverage was provided to the recipient and at least one other covered individual, while Code “2C” indicates that the coverage was provided through a marketplace.
Exemptions: If you or any of your covered individuals qualify for an exemption from the individual mandate penalty, Form 1095-B will include a code in Part III that indicates the exemption code. The instructions provide a list of exemption codes and their corresponding explanations.
Filing Requirements: The Form 1095-B instructions also provide information on how to use the information on the form when filing your tax return.
You will need to report information from Form 1095-B on your Form 1040, Form 1040A, or Form 1040EZ, depending on which tax return you are filing. You may also need to attach Form 1095-B to your tax return as proof of your health insurance coverage.
Corrections: If you receive a Form 1095-B with incorrect information, you should contact the entity that provided the form to request a corrected form. If you do not receive a corrected form in time to file your tax return, you can use other documentation to provide proof of your health insurance coverage, such as insurance cards or policy statements.
Importance of Form 1095-B: It’s important to note that although Form 1095-B is not required to be attached to your tax return, it is an important document that provides proof of your health insurance coverage.
The information on Form 1095-B is used to reconcile any premium tax credits you may have received to help pay for your health insurance coverage through a Marketplace, and to determine whether you may owe an individual mandate penalty.
Form 1095-B Recipient Guide
As a recipient of healthcare coverage, it’s important to be familiar with various tax forms related to your health insurance.
One such form is Form 1095-B, also known as the Health Coverage Form. In this article, we will provide an overview of Form 1095-B, including what it is, why you receive it, and how to use it.
What is Form 1095-B?
Form 1095-B is a tax form that provides information about your health insurance coverage for the previous year.
It is issued by insurance providers, including insurance companies, government agencies, and self-insured employers, who are required to report certain information about the coverage they provide. The form is sent to you, the recipient, as well as to the Internal Revenue Service (IRS).
Why do you receive Form 1095-B?
Under the Affordable Care Act (ACA), also known as Obamacare, individuals are required to have minimum essential health insurance coverage or face a penalty. Form 1095-B helps you and the IRS determine if you had the required coverage or if you qualify for an exemption.
Form 1095-B provides information about the type of coverage you had, the duration of the coverage, and the individuals covered under the policy. It also includes information about the insurance provider, such as their name, address, and taxpayer identification number (TIN).
This information is used by the IRS to verify that you had qualifying health insurance coverage or determine if you owe a penalty for not having coverage.
How to use Form 1095-B
Form 1095-B is an important document that you may need to use when filing your federal income tax return. Here’s how you can use it:
Review the information: Carefully review the information on Form 1095-B to ensure that it is accurate. Check the names, Social Security numbers, and other details of the individuals covered under the policy. Make sure that the coverage dates match the months in which you had coverage.
Keep it for your records: Keep a copy of Form 1095-B for your records. While you do not need to submit the form with your tax return, you may need to provide it as proof of your health insurance coverage in case of an IRS audit or if you receive an inquiry from the IRS.
Use it when filing your tax return: When you file your federal income tax return, you will need to indicate whether you had health insurance coverage for the year.
You will also need to report any exemptions you qualify for or calculate any penalties you owe if you did not have coverage. Form 1095-B can help you provide accurate information when completing these sections of your tax return.
Contact your insurance provider for corrections: If you find any errors on Form 1095-B, contact your insurance provider to request a corrected form. It’s important to ensure that the information reported on the form is accurate, as errors could result in delays or issues with your tax return.
What to do if you did not receive Form 1095-B
If you did not receive Form 1095-B, it does not necessarily mean that you did not have health insurance coverage. While insurance providers are required to send Form 1095-B to recipients, there may be situations where you are not required to receive the form, such as if you had coverage through Medicare or Medicaid.
If you believe that you should have received Form 1095-B but did not, contact your insurance provider to request a copy. You can also check your online account with your insurance provider, as they may have made the form available electronically.
Read Also: State Farm Drive Safe and Save: A Smart Way to Save on Car Insurance
Form 1095 Reporting Requirements
As part of the Affordable Care Act (ACA), also known as Obamacare, employers and health insurance providers are required to report information about the health insurance coverage they offer to employees or provide to individuals.
This information is reported on Form 1095, which is used to verify that individuals and their family members had minimum essential health insurance coverage during the year, as required by the ACA. Here’s what you need to know about Form 1095 reporting requirements.
What is Form 1095?
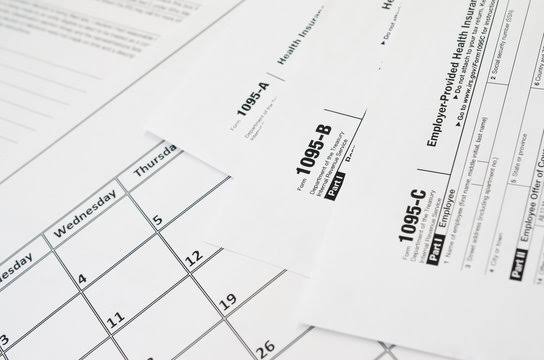
Form 1095 is a series of forms used for reporting health insurance coverage information to the Internal Revenue Service (IRS) and to individuals who are covered by the health insurance. There are three types of Form 1095:
Form 1095-A, Health Insurance Marketplace Statement: This form is used by individuals who enrolled in health insurance coverage through the Health Insurance Marketplace, also known as the Exchange. It provides information about the coverage, premium amounts, and any premium tax credits or other financial assistance received.
Form 1095-B, Health Coverage: This form is used by insurance providers, such as insurance companies, government agencies, and employers who are not considered applicable large employers (ALEs), to report information about the health coverage they provide.
It includes details about the covered individuals, the months of coverage, and any premium payments made.
Form 1095-C, Employer-Provided Health Insurance Offer and Coverage: This form is used by applicable large employers (ALEs), which are employers with 50 or more full-time employees, including full-time equivalent employees, to report information about the health insurance coverage they offer to their employees.
It includes information about the employees, the months of coverage offered, and the affordability of the coverage.
Who Must File Form 1095?
Under the ACA, employers and health insurance providers are required to file Form 1095 if they offer minimum essential coverage to individuals. This includes:
Applicable Large Employers (ALEs): Employers with 50 or more full-time employees, including full-time equivalent employees, are considered ALEs and are required to file Form 1095-C. ALEs must also provide a copy of Form 1095-C to each of their full-time employees, regardless of whether the employee enrolled in the offered health insurance coverage or not.
Providers of Minimum Essential Coverage: Health insurance providers, including insurance companies, government agencies, and self-insured employers, are required to file Form 1095-B to report information about the health coverage they provide.
This includes coverage offered to individuals and their family members, regardless of whether the coverage was obtained through the Health Insurance Marketplace or not.
It’s important to note that if an employer or health insurance provider is part of a controlled group or an affiliated service group, they may be considered an ALE based on the combined number of employees in the group.
When to File Form 1095?
The deadline for filing Form 1095 with the IRS varies depending on the type of form and whether the employer or health insurance provider is filing electronically or by paper.
For electronic filing: Form 1095-B and Form 1095-C must be filed with the IRS by March 31st of the year following the calendar year for which the information is being reported.
For paper filing: Form 1095-B and Form 1095-C must be filed with the IRS by February 28th of the year following the calendar year for which the information is being reported.
In addition to filing with the IRS, employers and health insurance providers must also provide a copy of Form 1095 to the individuals who are covered by the health insurance.
Read Also: Elephants (Elephantidae): Species, Facts, Habitat, Diet, etc.
